Introduction
Kidney disease, also known as renal disease or nephropathy, refers to damage or dysfunction of the kidneys that impairs their ability to filter waste and excess fluids from the blood. Maintaining kidney health is crucial as these organs play a vital role in regulating bodily functions, including waste removal, electrolyte balance, and blood pressure control. Buy Real kidney here
Types of Kidney Disease
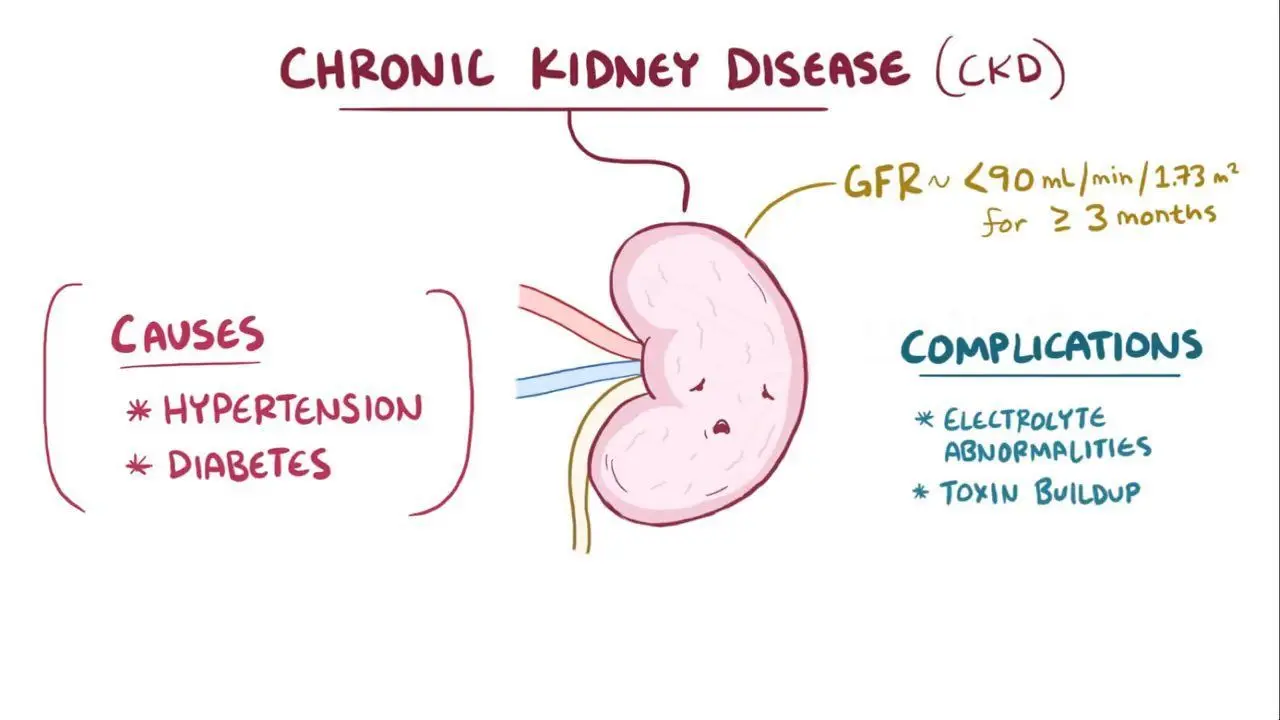
- Chronic Kidney Disease (CKD): A progressive loss of kidney function over time, often due to underlying conditions such as diabetes and hypertension. CKD can lead to end-stage renal disease (ESRD), where dialysis or transplantation becomes necessary.
- Acute Kidney Injury (AKI): A sudden reduction in kidney function that can occur over a short period, often due to factors like dehydration, infection, or exposure to nephrotoxic substances.
- Polycystic Kidney Disease (PKD): A genetic disorder characterized by the growth of numerous cysts in the kidneys, which can lead to kidney failure.
- Glomerulonephritis: An inflammation of the kidney’s filtering units (glomeruli) that can result from infections or autoimmune diseases.
- Diabetic Nephropathy: A complication of diabetes that damages the kidneys’ filtering system over time.
Causes
- Diabetes: High blood sugar levels can damage the kidneys’ filtering system.
- Hypertension: Chronic high blood pressure can strain the kidneys and impair their function.
- Genetic Factors: Conditions like PKD are inherited and can predispose individuals to kidney disease.
- Infections: Recurrent infections can lead to kidney damage.
- Environmental Factors: Long-term exposure to certain toxins and medications can adversely affect kidney health.
Warning Signs and Symptoms
- Fatigue: General tiredness due to toxin buildup.
- Swelling (edema): Fluid retention causing swelling in hands, feet, and face.
- Changes in Urination: Increased frequency or reduced output of urine.
- Nausea and Vomiting: Resulting from toxin accumulation in the body.
- Shortness of Breath: Fluid buildup in the lungs can lead to breathing difficulties.
If your kidney function continues to decline, you may start developing symptoms of kidney disease. Each person is different, but most people will start to develop uremia as the kidneys fail and are unable to remove wastes from the body. There are many symptoms of uremia that occur as kidney function declines, including:
Weight loss
Weakness
Vomiting
Loss of appetite
Shortness of breath
Leg cramps
Itching
Chest pain
Easy bruising
Swelling in ankles and legs
Fatigue
Nausea
Bad taste in the mouth
Restless legs
Forgetfulness
Difficulty sleeping
Cold intolerance
Skin colour changes
Decreased sexual desire
Are You At Risk?
Did you know that 1 in 10 Canadians has kidney disease? Take 10 minutes to answer these 10 questions. The answers will help you know if you should talk to your doctor about having your kidney function checked. Buy Real kidney here
Diagnosis
Diagnosis typically involves:
- Medical History Review: Evaluating risk factors and symptoms.
- Blood Tests: Measuring creatinine levels and estimating glomerular filtration rate (GFR).
- Urine Tests: Checking for protein or blood in the urine.
- Imaging Tests: Ultrasound or CT scans to assess kidney structure.
- Kidney Biopsy: A procedure to obtain tissue samples for further examination.
Treatment Options
- Lifestyle Changes: Dietary modifications, weight management, and regular exercise can help manage symptoms and slow progression.
- Medications: Drugs may be prescribed to control blood pressure, manage diabetes, or treat underlying conditions.
- Dialysis: A procedure that artificially removes waste products from the blood when kidneys fail.
- Kidney Transplant: Replacing a failed kidney with a healthy one from a donor.
Prevention
Preventive measures include:
- Healthy Diet: Low in salt and processed foods to support kidney health.
- Regular Exercise: Maintaining a healthy weight and improving overall health.
- Managing Chronic Conditions: Keeping diabetes and hypertension under control.
- Avoiding Nephrotoxic Substances: Limiting exposure to drugs and chemicals harmful to kidneys.
Detection
Sometimes even people with serious kidney disease have no symptoms. That is why a blood or urine test is necessary to check for kidney problems.
There are two key tests used to detect kidney damage and to assess how well your kidneys are functioning at removing toxins and waste products from your blood.
Blood test
A blood test is used to measure your serum creatinine level which helps to indicate how well the kidneys are filtering the blood. Creatinine is a waste product made from muscle use and the breakdown of the protein you eat. As the blood creatinine rises, kidney function decreases. Decreased kidney function means that your kidneys are not able to remove the toxins and waste products from your blood as well as someone with normal kidney function.
The estimate (or percentage) of kidney function is called the glomerular filtration rate (GFR) or estimated glomerular filtration rate (eGFR). Glomeruli are tiny blood vessels in the kidney that help to filter waste. The GFR is a way of measuring how well the kidneys are working by determining the rate at which the glomeruli are filtering waste products from your blood. The eGFR is the most common way to measure kidney function at kidney clinics. Buy Real kidney here
Urinalysis
Simple laboratory tests such as urinalysis (a urine dipstick), which looks for blood and a protein called albumin in the urine, are also useful in detecting kidney damage at an early stage and determining your risk of losing more kidney function. The filters of the kidney do not normally allow protein in the urine so if protein (albumin) is detected, it is a sign that the filters of the kidney are being damaged. The more albumin that you have in your urine, the greater the risk of losing kidney function over time. Other blood tests, X-rays, kidney ultrasound or a kidney biopsy may also be needed to diagnose the specific type of kidney disease and to determine the appropriate treatment.
Risk Factors
There are a number of risk factors for kidney disease, some that you can control such as smoking, and others that you cannot. People with diabetes, high blood pressure or who have a family history of kidney disease are at increased risk, as well as children born with kidneys that did not develop properly.
People of Aboriginal, Asian, South Asian, Pacific Island, African/Caribbean and Hispanic descent are also at higher risk, but you may develop kidney disease even if you do not fall into one of these groups.
Be very careful about taking non-prescription medications, particularly painkillers. It is wise to discuss all over-the-counter medications with a doctor or pharmacist before they are taken. Certain other medications, toxins, pesticides and illegal drugs (such as heroin and cocaine) can also cause kidney damage.
Recent estimates suggest that as many as two million Canadians have chronic kidney disease or are at risk — most are unaware of it. If you are over the age of 50 or fall into any of the aforementioned risk categories ask your doctor for a blood test to know your kidney function level.
Conclusion
Kidney disease significantly impacts individuals’ health and quality of life. Early detection through regular check-ups is vital for effective management and prevention of progression to more severe stages. Understanding the importance of kidney health can lead to better outcomes through proactive lifestyle choices and medical interventions.